
hepatitis
(liver inflammation)Introduction
The term ‘hepatitis" implies an inflammation and impaired function of the
liver. There are many causes of hepatitis including several infectious
agents, toxic substances including alcohol and medicines, and mechanical
blockages of the drainage system of the liver. Most commonly, the
layperson’s use of the word hepatitis implies one of the infectious
diseases caused by several different viruses. Our discussion of this
subject is confined to a few of the more common infectious causes.
Anatomy and Physiology of the Liver
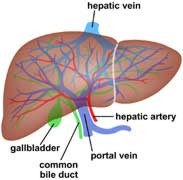
The liver is a large organ
located in the upper right quadrant of the abdomen. Tremendous amounts of
blood pass through the liver to be filtered and detoxified. In broad
terms, the liver is similar to a recycling centre for the body. The liver
and kidney process most of the blood-borne toxins in the body and either
eliminate the hazards or convert them into a less hazardous form. The
liver eliminates hazards and passes them into the stool, while the kidney
eliminates hazards into the urine. Most medications are "metabolized" or
changed to a different form in the liver. These different forms may be
either more active or less active than the original form.
The liver also processes nutrients and assists in the conversion of food
to nutrients. In this role, the liver may convert sugars into more complex
substances to be used slowly by the body using insulin. It also converts
dietary cholesterol and fats into the healthy and unhealthy forms of
cholesterol. The liver aids in fat digestion by producing bile which is
stored in the adjacent gall bladder. The liver is an essential organ for
daily functioning of the body.
Viral Infections of the Liver
Small virus particles may infect the liver and impair its ability to
function. When this occurs, individuals may feel acutely fatigued,
feverish, nauseated and lose their appetite. The urine may become very
dark as the body tries to excrete a breakdown product of blood called
bilirubin through the urine instead of the normal pathway through the
liver and into the stool. The skin may turn yellow (jaundice) due to
bilirubin deposition in the skin. In addition to the illness caused in the
individual by hepatitis, a significant danger lies in its transmissibility
to other people. Chronic forms of hepatitis may develop that lead to liver
failure and liver cancer. There are many forms of infectious hepatitis.
The most common are Hepatitis A, Hepatitis B and Hepatitis C.
Hepatitis A
Hepatitis A infects approximately 180,000 people in the US each year. Of
the US population, 33% will be infected during their lifetime. The virus
is found in contaminated food, water, milk and shellfish. It is primarily
related to overcrowding, poor sanitation and poor personal hygiene.
Contamination occurs when the virus excreted in the stool of an infected
individual gets into drinking water or food. The most common scenarios
occur with poor water processing facilities and poor hand washing in
preparing food. A single individual can infect hundreds of people in a
very short period of time. Major outbreaks have recently occurred in the
US. Raw seafood, particularly oysters, which concentrate wastes dumped
into the ocean, may also transmit the condition without being directly
handled by an infected individual.
Hepatitis A may range in severity from almost no symptoms to being very
ill. Symptoms include fatigue, fever, chills, headaches, nausea, vomiting,
weight loss, jaundice, and darkened urine as discussed earlier. The
condition is usually not fatal in otherwise healthy individuals. Symptoms
occur from 15 to 45 days after the exposure to the virus. The symptoms
usually last from one to two weeks with complete recovery within two
months. There is no specific treatment other than supportive care and
avoiding liver toxins such as alcohol. Even some over the counter
medications such as Tylenol should generally be avoided. Once recovery is
complete, the individual gains some immunity against future infection by
that strain of virus.
Very rarely, death results from a fulminant infection. The diagnosis is
made by testing the blood for antibodies to the hepatitis A virus and
followed by monitoring blood enzymes from the liver. Elevated liver
enzymes generally return to normal as the individual recovers, although
this is not always the case.
Hepatitis B
Hepatitis B is a blood borne infection transmitted through contaminated
body fluids. It affects 0.1% to 0.5% of low risk people in the US
(128,000+ annually) and 200 million individual worldwide. Hepatitis B is
the primary cause of liver cancer worldwide and is responsible for more
cancer deaths than any other agent in the third world. In areas that have
adopted Western lifestyles, it is less prevalent and cigarettes are a much
more common cause of other fatal cancers. People at risk for Hepatitis B
include intravenous drug users, those with high-risk sexual behavior,
infants of mothers with hepatitis and health care workers exposed to
infected blood and body fluids. Blood used for transfusion in the US is
screened for infectious hepatitis.
Hepatitis B also has a wide range of symptoms, but is a potentially much
more serious disease than hepatitis A. Up to 10% of infected people, over
one million in the US, develop a chronic infection that is contagious (90%
of infected infants). This condition also puts the individual at risk for
hepatic carcinoma (liver cancer). A small percentage of people develop
chronic, active hepatitis, a situation where recovery is incomplete. This
may require long term treatment with medication that is poorly tolerated
in some and may disqualify a pilot or controller from aviation duties.
Finally, approximately 0.1-1.0% develop "fulminant hepatitis", a very
aggressive and often fatal form of the disease. Nearly 6,000 deaths per
year in the US are attributable to hepatitis B.
Hepatitis C
Hepatitis C is a relatively newly discovered form of liver disease that
has recently received considerable public attention and media coverage.
The virus was not discovered until 1988 and reliable testing did not exist
until 1992. Unfortunately, the virus has infected many people prior to
that time. Approximately four million Americans (2 percent of the
population) are infected with hepatitis C and 10,000 will die of the
disease each year. The current medical costs in the US associated with
treating the disease are over $600 million annually.
Worldwide, 170 million people are infected. Hepatitis C is transmitted
through contaminated blood and body fluids, similar to Hepatitis B.
High-risk behaviours such as intravenous drug use and unprotected
intercourse with infected individuals accounts for most of the
transmission. Blood transfusions prior to improved testing of the blood
supply prior to 1992 accounts for about 7% of the infections.
The clinical picture of hepatitis C, at least in the early stages, is
quite different from Hepatitis A or B. Unlike the latter two, people
infected with hepatitis C rarely have any symptoms for 10-30 years. They
appear perfectly healthy, yet carry the disease and can infect others.
Approximately 80% of people infected will develop chronic inflammation of
the liver in 10-30 years and 20% will develop cirrhosis which destroys the
liver, resulting in the need for a liver transplant to prevent death.
Other forms of hepatitis due to viruses include Hepatitis D, E and G.
Transmission for most is similar to hepatitis B through infected blood.
Hepatitis E is transmitted by contact with infected stool similar to
Hepatitis A.
Prevention of Hepatitis A
Fortunately, prevention of these diseases is usually easy to accomplish.
Exceptions can occur when hepatitis A contaminated food is unsuspectingly
consumed in an area where transmission risk is usually very low (e.g.
North America or Western Europe). When travelling to areas with poor
hygiene, using the same steps one would use to avoid traveller's diarrhoea
are fairly effective in preventing hepatitis A.
You should avoid uncooked foods and only eat fruits and vegetables that
you personally peel. Avoid water or ice. Even "bottled" water may be
contaminated if not obtained from a reliable clean source. In the past,
people travelling to high risk areas were given "gamma Globulin" or immune
serum globulin which gave a partial temporary immunity. These painful
shots conveyed passive immunity, a transient protection gained from other
infected persons’ serum.
Recently, vaccines for hepatitis A (Havrix and Vaqta) have been developed.
They are much more effective in conveying a lifelong active (produced by
your own body) immunity. The vaccine series is given as a two shot series
with the second shot given 6 months after the first for adults.
Significant immunity occurs within several weeks of the first
immunization. These shots are usually very well tolerated and relieve the
need for repeated painful gamma globulin injections. See the Practice
Guidelines recommendations of the Advisory Committee on Immunization
Practices for prevention of Hepatitis A.
For those individuals travelling to high risk areas, the vaccine is highly
recommended. Information concerning high risk areas of the world may be
obtained from the Centres for Disease Control and Prevention.
If an individual is infected with hepatitis A, household contacts should
consider immunization and administration of immune globulin. Excellent
personal hygiene and avoiding food preparation significantly decrease the
risk of transmitting the disease.
Prevention of Hepatitis B
Immunizations for hepatitis B (Engerix-B and Recombivax-HB) are also
available in a three shot series given as an initial dose followed by
doses at one and six months. For those not engaging in high-risk
behaviour, the risk of acquiring the disease is not significant. Those who
may be exposed to blood or body fluids of infected persons, usually
through sexual contact, should receive the immunization series.
Chronically infected individuals may benefit from treatment with
interferon. The treatment requires frequent injections and is often
accompanied by a flu-like syndrome. This treatment must be reported to and
generally is not cleared by the FAA for safety sensitive duty.
Prevention and
Treatment of Hepatitis C
Currently, no vaccine exists for hepatitis C. Prevention, therefore, is
limited to avoiding blood an body fluids of infected individuals. The
blood supply is now tested for hepatitis C, but those individuals who
received blood transfusions prior to 1992 may consider getting a simple
blood test to screen for the disease. Those who are infected should avoid
substances that may harm the liver, particularly alcohol, but also some
medications. Some people advocate nutritional therapy to boost the immune
system, though this has not been studied enough to be of proven to be of
benefit.
Symptomatic people infected with hepatitis C may benefit from treatment
with interferon-alpha and ribavirion, a recently approved FDA combination
for the condition named Rebetol. The treatment is expensive and only
improves symptoms in some individuals. It does not cure the disease and
has significant side effects of fatigue, fever, muscle aches and flu-like
symptoms.
The FAA briefly changed its policy and for several months allowed
certification of pilots using alpha interferon for the treatment of
hepatitis C. However, in late September 2001, the FAA reversed its earlier
position because of concerns about depression secondary to use of alpha
interferon. Currently, no forms of alpha interferon are approved for
medical certification.
FAA Policies Regarding Hepatitis
The acute forms of hepatitis are disqualifying for aviation duties. If the
condition resolves spontaneously, an individual may return to flying after
clearance from the treating physician and when the pilot feels confident
they can perform all of their required duties. This condition may be
reported to the FAA at the time of the pilot's next FAA physical
examination. Controllers must clear through the Regional Flight Surgeon
before returning to safety sensitive duties.
Chronic hepatitis conditions requiring the use of medication must be
cleared by the FAA prior to exercising the privileges of the aeromedical
certificate. Certification is dependent upon minimal symptoms from the
disease and tolerance of the medications. Periodic reports from the
treating physician are required for continued certification. See an
article in the Fall 2003 Federal Air Surgeon's Medical Bulletin, "Medical
Certification in a Student Pilot With Hepatitis C Infection".
Summary
Hepatitis is a term covering a broad spectrum of diseases affecting the
liver. Infectious forms of hepatitis are relatively common and can cause
serious illness and death. Prevention is the key to avoiding the
consequences of the disease. Medical certification of pilots/controllers
with hepatitis depends on the seriousness of the disease and the method of
treatment. Those pilots/controllers whose disease is well controlled, and
who tolerate medication well, may be medically certified by the FAA after
review and approval of appropriate medical documentation. Numerous
credible resources for additional information on hepatitis exist.
|
