
kidney stones
Introduction
Kidney stones afflict over 500,000 Americans each year. Approximately 10%
of the US population will get kidney stones in their lifetime. The pain
from these stones can be excruciating and incapacitating. Nearly 60% of
people with kidney stones will have a recurrence within ten years of the
first stone. The presence of a kidney stone is generally disqualifying for
FAA aeromedical certification. Once the pilot/controller is stone free,
flying duties may resume after clearance from the AME or the FAA.
Controllers also have to be cleared by the Regional Flight Surgeon. Under
certain circumstances, pilots and controllers with retained kidney stones
may also be cleared by the FAA to return to safety sensitive duties. In
the year 2004, the physicians of Virtual Flight Surgeons, Inc. assisted
nearly 350 pilots/controllers with kidney stones return to flying related
duties.
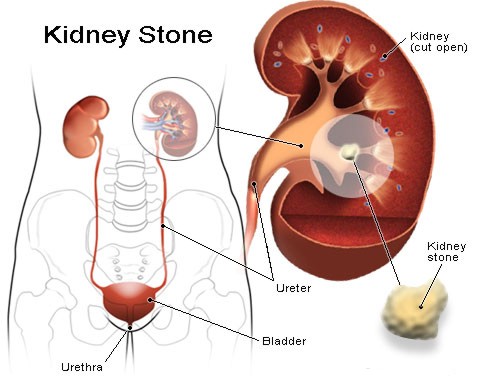
Renal Anatomy
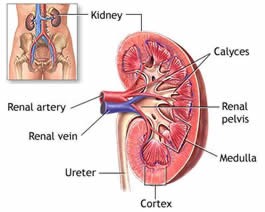
The anatomy of the urinary
system has four main components, the kidneys, the ureters, the bladder and
the urethra. Urinary stone disease encompasses several types of stones
found in several locations, though the common term for all of the
locations is "kidney stones".
Renal stones are located in the kidney. Calyceal stones are found in the
funnel shaped area called the calyx between the kidney and the ureter.
Ureteral stones are in the tube that drains urine from the kidney to the
bladder. Stones are usually most painful when they migrate down, or are
lodged in, the narrow part of the ureter. The narrowest area of the ureter
is that portion that extends into the bladder, also known as the
ureterovesicular junction or UVJ. Stones in the bladder do not usual cause
symptoms unless they become lodged in the prostatic or penile urethra.
"Saddle" stones extend from the calyx into several portions of the kidney
and rarely pass spontaneously.
Composition of Stones
Stones are made up of
several different substances. Most stones are made of calcium oxalate,
calcium urate or calcium pyrophosphate. Occasionally, stones are made of
primarily uric acid, cysteine or struvite. Calcium stones are usually
visible on x-rays, while uric acid stones are nearly invisible. The
composition of the stones is important in locating the stones and deciding
how to treat recurrent stones. Stone composition is determined by sending
a stone strained from the urine for chemical analysis. A 24 hour urine
collection can also be analyzed and compared to blood chemistries to
determine if the kidney is excreting too much or too little of a compound
leading to increased risk for stone formation. Kidney function is also
measured using 24 hour urine analysis called creatinine clearance.
Symptoms and Diagnosis of Kidney Stones
Urinary stones usually manifest as severe, acute pain on one flank or the
lower back. Pain may radiate into the scrotum or testicle on the same side
for men, and into the groin area of the same side for women. Urinalysis
may show microscopic blood that is not visible to the naked eye.
Occasionally, a stone without any pain is detected after a urinalysis
shows blood or an x-ray that is taken for another reason shows a stone.
The diagnosis of a stone is often done with an x-ray. Some small stones
are often difficult to find even if the physician is specifically looking
for the stone. An Intravenous Pyelogram (IVP) involves injecting a dye
that is visible by x-ray and excreted by the kidneys. The IVP shows an
outline of the kidneys, calyces and ureters. If a stone is blocking the
ureter, the dye swells the ureter above the stone and may not pass into
the ureter below the stone.
At times, Computerized Tomography (CT) scans are used to locate stones,
particularly smaller stones that may not be visible on x-ray films.
Later evaluation of the cause of the stone may involve a 24 hour
collection of urine to determine the concentration of certain chemicals
known to provoke stone formation.
Treatments for Kidney Stones
Many treatments exist for stones. The FAA does not dictate a particular
treatment for stones, so any treatment agreed to by the pilot/controller
and the physician that results in elimination of the stone is waiverable
for return to flying/controlling. As discussed above, the most
conservative treatments involve the spontaneous passage of the stone after
oral or intravenous hydration. Adequate hydration by generous fluid intake
is also a key element in the prevention of kidney stones.
Medical Treatment
Medical treatment for stones involves the increasing of the urine output
and pain relief. People with stones are instructed to drink large amounts
of fluids (one or more gallons) a day in an attempt to flush the stone
through the urinary system. For those who may have enough pain to cause
nausea and vomiting, an IV may be used to provide large amounts of fluids.
Pain relief may require narcotics, especially as the stone moves down the
ureter.
Extracorporal Shock Wave Lithotripsy (ESWL)
Stones of a certain size range located high in the urinary system that may
not pass spontaneously are candidates for extra-corporal shockwave
lithotripsy (ESWL). This procedure uses sound waves from several sources
outside the body focused on the stone to fragment it into smaller pieces
that can pass spontaneously. There are several techniques for lithotripsy.
The procedure requires anaesthesia and many patients report considerable
soreness after the ESWL. Often a stent, or hollow tube, is inserted into
the ureter using a scope inserted through the bladder. The stent is to
decrease the pain of the residual gravel from the shattered stone passing
through the ureter. After all the fragments have passed, the stent is
removed. Recovery and stone passage may take several days to weeks.
Ureteroscopic Stone Removal (Basket Extraction)
Stones located lower in the collecting system (closer to the bladder) may
be removed by a basket extraction technique. A probe is inserted through
the urethra and bladder into the ureter. Using direct visualization of a
fiberoptic scope, the stone is grabbed and surrounded by a clasp or
expandable cage (basket) and manipulated through the probe. The entire
probe is removed dragging the stone out with the probe. Recovery is
usually within several days. As with the ESWL, a stent is sometimes left
in place in the ureter for several days to allow healing. Not all stones
are located in areas where this technique is practical.
Percutaneous Nephrolithotomy
A more invasive procedure is the percutaneous nephrolithotomy. This is
usually reserved for stones in the kidney or calyx that are too large to
pass and too large for ESWL. An small incision through the back and into
the ureter is made to directly visualize the stone through a small scope.
The stone is then removed through the scope. Sometimes the stone must be
broken up to remove through the scope. The recovery time is somewhat
longer for this procedure and may require several days hospitalization. As
in the above procedure, the advantage over ESWL is that the stone is
removed rather than passing through the ureter.
Medications
If evaluation of the cause of stone formation reveals abnormal
concentrations of certain substances in the urine or blood, medication may
be prescribed to change the concentration and lower the risk of recurrent
stone formation.
Medication to prevent recurrences of kidney stones includes the diuretic
hydrochlorothiazide (HCTZ) which decreases calcium excretion in to the
urine. Allopurinol (Zyloprim) is used to decrease uric acid production by
the body and hence lower the concentration in the urine. Both medications
are waiverable by the FAA after an observation period free of side
effects. Since HCTZ lowers blood pressure and causes potassium loss, the
FAA may require periodic reports including blood tests for potassium (K+)
on future medical applications. Other medications may be prescribed to
change the acidity or alkalinity of the urine and decrease the risk of
stones. These are also waiverable.
Prevention of Kidney Stones
Prevention of stones is best accomplished by maintaining hydration. The
dry environment of the pressurized aircraft cabin predisposes to
dehydration. A lack of a ready source of fluids and an unwillingness to
frequently leave the cockpit to "attend to physiologic needs" during long
flights also puts the pilot at increased risk for dehydration and stone
formation. The commuter pilot who has little time between flights, often
sits on a hot tarmac and has physical work to perform associated with the
flight may also get dehydrated. The general aviation pilot on a long cross
country without sufficient water carried on board is also at risk. The
body is usually a liter dehydrated before an individual becomes thirsty. A
good rule of thumb is to drink enough to keep the urine clear. Pilots with
previous kidney stones rarely forget this rule.
Certain medications, such as Crixivan, are known to cause stones in some
users. Certain foods that contain purines, oxalate or calcium may place
individuals at risk. Foods high in oxalates include rhubarb, asparagus,
spinach, chocolate, tea and coffee. Foods high in purines include organ
meats (liver, brain), sardines, beans, beer and red wine. Not all people
will benefit from restricting these foods, however. A 24 hour urine
collection and analysis will aid your physician in recommending whether or
not to restrict certain foods. If stones are composed of calcium oxalate
or calcium phosphate, the use of a medication, hydrochlorothiazide, may
reduce the risk of recurrence. Risk of recurrence of stones of uric acid
may be reduced by the use of allopurinol. Allopurinol is sometimes used
with calcium oxalate stones as well.
FAA Policy on Flying/Controlling After Kidney Stones
The FAA will certify a pilot/controller who has had a single episode of
kidney stones to fly after all stones are cleared, the individual is
stable and documentation is forwarded to the FAA for clearance. Many AME’s
are willing to clear a pilot also, if they have the appropriate
documentation. The documentation should include reports of the evaluation
and treatment, as well as a report of x-ray confirmation that the
pilot/controller is stone free. Controllers do require specific clearance
from the Regional Flight Surgeon prior to returning to controlling. The
following criteria must usually be met:
1) Radiographically stone free
2) Normal renal function,
3) No evidence of metabolic stone disease.
Individuals with recurrent episodes of kidney stones are required to
present information to the FAA that they are free of stones before
returning to aviation duties. This is a recent change in FAA policy
effective September 2003. Recurrent episodes generally require a 24 hour
urine analysis as well.
For those pilots/controllers who have retained stones that do not pass,
the FAA will consider granting a waiver if their physician can affirm that
the stone appears stable and is unlikely to pass spontaneously. Stones
greater than 2 mm in size or those located in the upper or mid calyces are
less likely to receive waivers. The hazard is that a retained stone may
pass during flight and compromise flying safety.
A recent change in the Guide to Aviation Medical Examiners indicates that
individuals with a history of retained stones may not be cleared to return
to flight duties by their AMEs after documenting they are stone free.
Instead, authorization must be obtained from the FAA Aeromedical
Certification Division (AMCD) or the Regional Flight Surgeon.
For the first episode of a stone, the FAA will not generally require
follow-up reports from the pilot or controller's personal physician on
subsequent FAA medical examinations. Those with a history of recurrent or
retained stones should expect to be required to submit these reports for
several years at the time of their FAA medical examinations.
kidney
disease and annual medical examinations
For the last thirty years I have been suffering from IgA nephritis and have
been under the care of a Nephrologist. My kidney function is now approx. 25% and
I am on medication which is controlling the symptoms well. My blood pressure on
the 9th August was 120/80. I am 55 years old and at my last medical the CAA only
allowed me to renew my certificate for one year instead of the usual two year
period.
I would like to appeal this ruling as I have complete and detailed checkups
every two months. I would be agreeable to supply regular details of these to the
Director Aviation medicine if this would save having to spend another $100 on a
medical in December 1995 which does not seem to me to be as detailed as the ones
already carried on a regular basis.
Do you consider this to be a reasonable proposition to put to CAA? If so would
AOPA assist me in this matter?
Your questions are more political than medical but I'll try my best.
You do have a significant kidney disease which has caused a considerable
reduction in the performance of your kidneys. The problems associated with this
kidney disease appear to be well controlled.
It is not unreasonable for CASA to want to keep a close eye on your medical
condition. The easiest way they have to do this is by requiring annual aviation
medical examinations. Annual aviation medical examinations will provide CASA
with the information they want but you might, quite reasonably, question the
cost / benefit aspects of this decision.
As I see it you have several options:
-
Negotiate with your DAME to see if they would be willing to fill out your
aviation medical forms for free during their routine follow-up of your kidney
condition. After all they are surely seeing you regularly enough to keep an
eye on your kidneys, it's not an unreasonable request that at least every
second aviation medical be provided at a significant discount;
-
Approach CASA's Office of Aviation Medicine with your proposal and explain
the hardship that their annual medical requirements place on you. They may not
accept your submission but they will be certain to give it full, individual,
consideration;
-
Accept CASA's requirement and find the extra $75 - $100 somehow;
-
Approach AOPA requesting their support in further lobbying CASA.
These options are listed in the order I see as most appropriate. Your DAME
might be very amenable to your approach and provide a discount for your
medicals. Failing that, CASA may modify their requirement after appropriate
representation from you. If that fails you will need to decide between finding
the extra funds and requesting further AOPA support in lobbying CASA.
In conclusion:
-
CASA has not been unreasonable in their wanting to keep a close watch on
your medical condition;
-
You are being similarly reasonable in questioning the cost / benefit
aspects of their decision;
-
A formal, AOPA supported, lobbying campaign should be your last resort.
Advice:
-
Speak with your DAME - Will they discount your medical examinations?
-
Write to CASA - Will they remove this requirement in light of the
financial hardship it causes you or will they accept alternative evidence of
your continued good health?
-
Be sure that the extra cost cannot be easily met and that you believe the
CASA stance is not reasonable;
-
Then, and only then, pursue a formal lobbying campaign of CASA.
|
